I am aware of mental health. I’m aware of Eating disorders, I’m aware of Autism and Tourette’s and Fibromyalgia, I’m even aware of Goths (yes, there is a Goth awareness day), and I’m very aware of how tired of awareness days I am. At the moment, there is (rightfully) a lot of focus on the mental health effects of the pandemic and lockdown; however, those of us who struggled before feel like we’ve been yelling about social isolation and the 9-5 lifestyle being detrimental to our mental health for years, but no one listened.
The thing about gaining awareness is that it’s meaningless. How do you quantify awareness? How do you evidence it? What exactly is the aim?. People with mental health problems are aware of helplines and Time to Talk campaigns, we’ve heard all the talk to someone messages, but who do we talk to? And what happens when talking isn’t enough? Or when no one listens?.
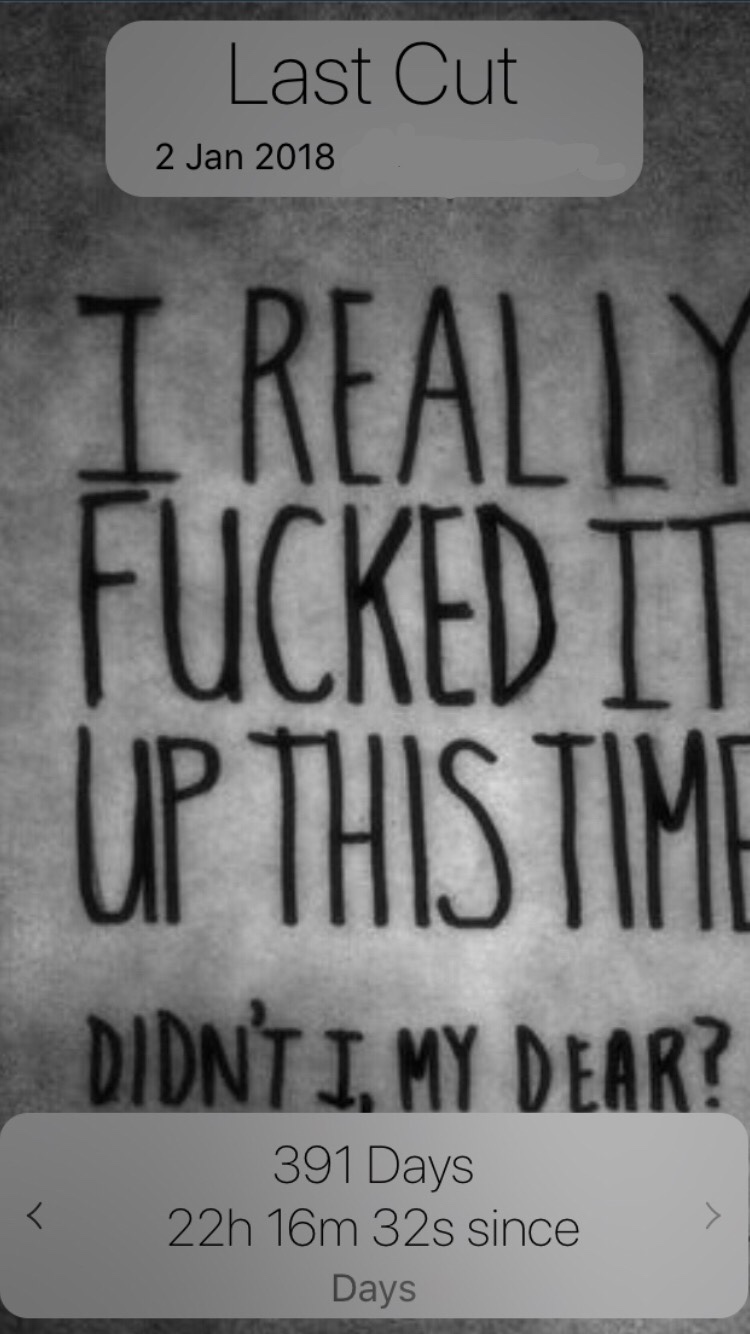
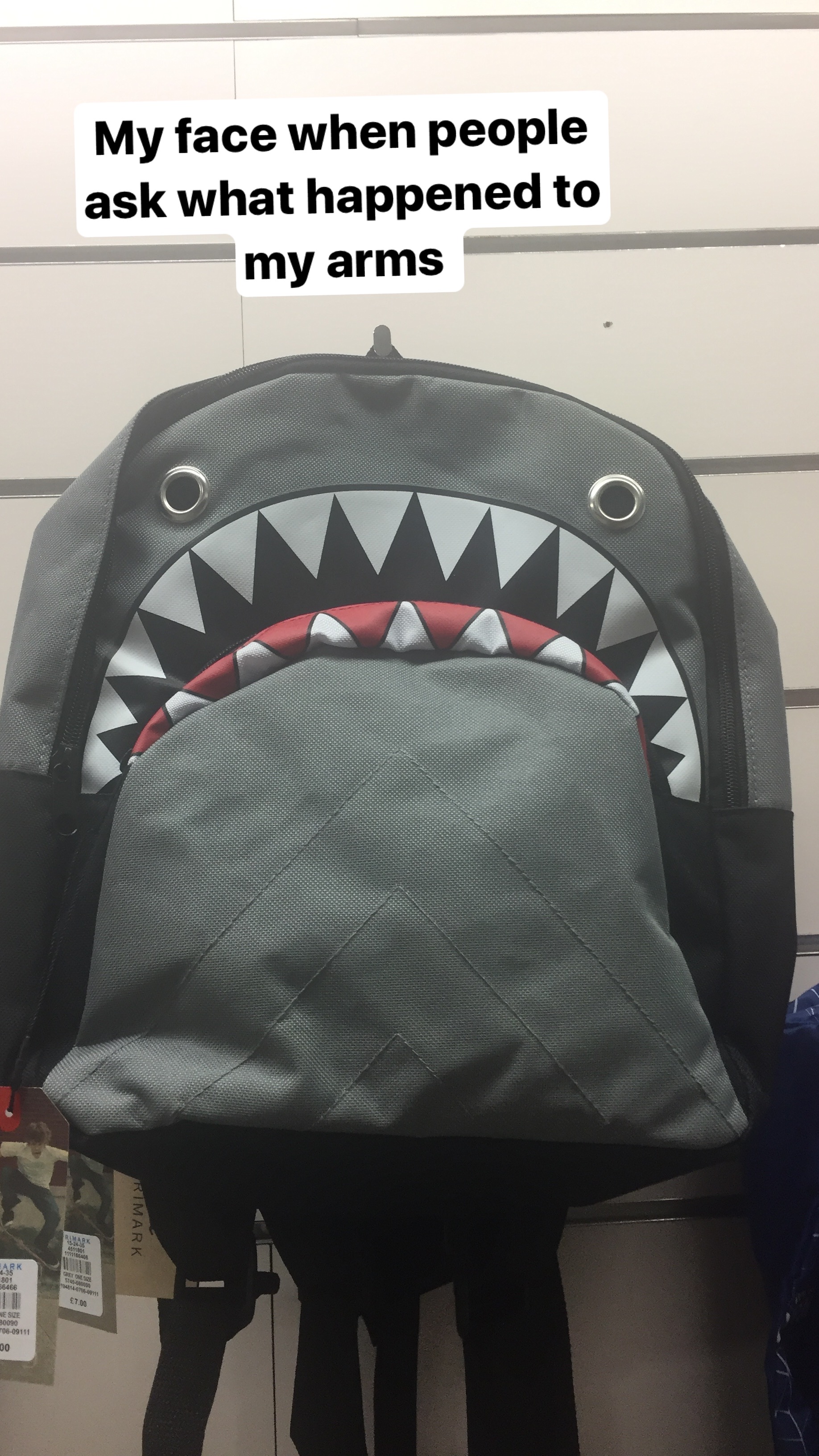
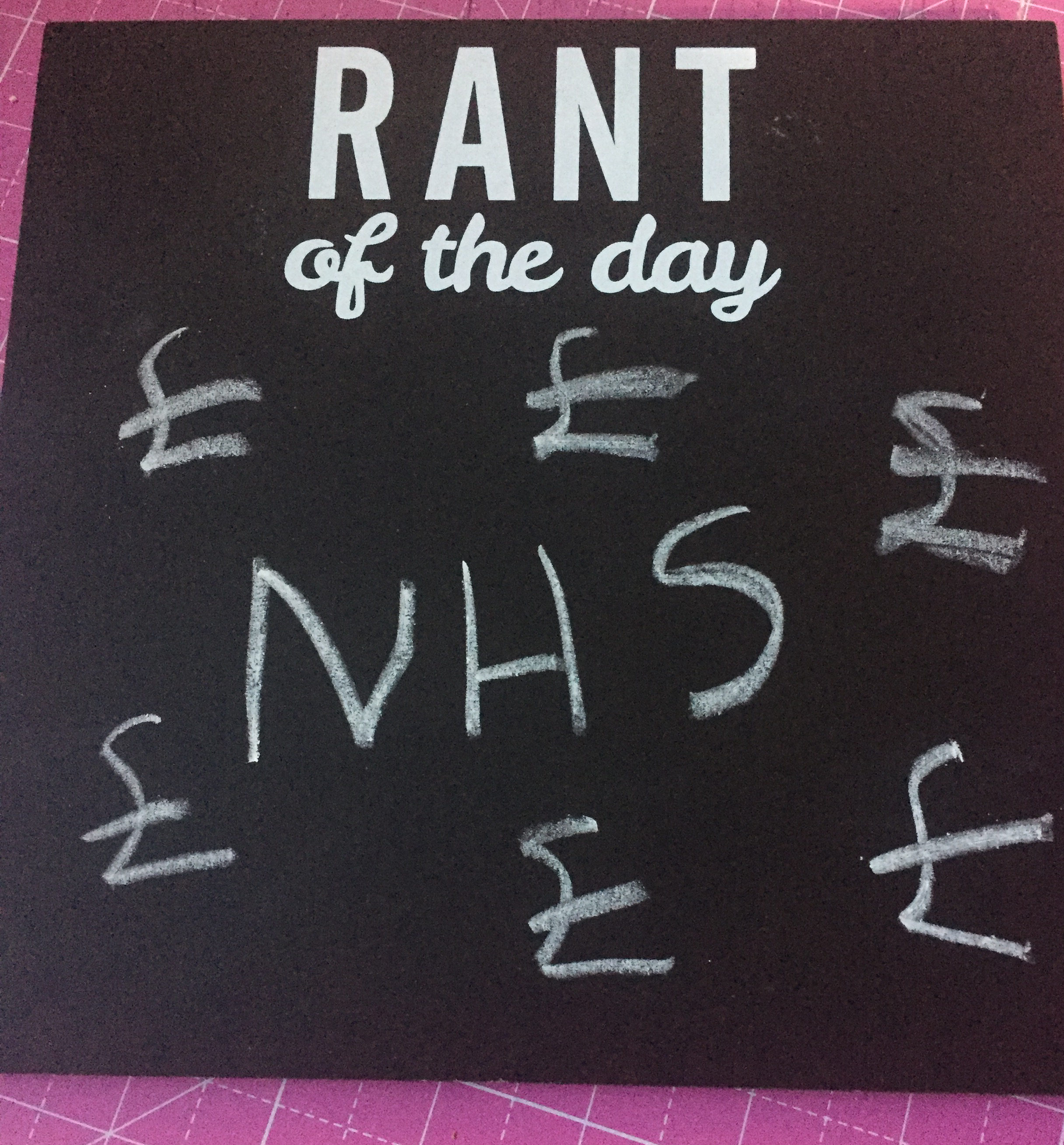
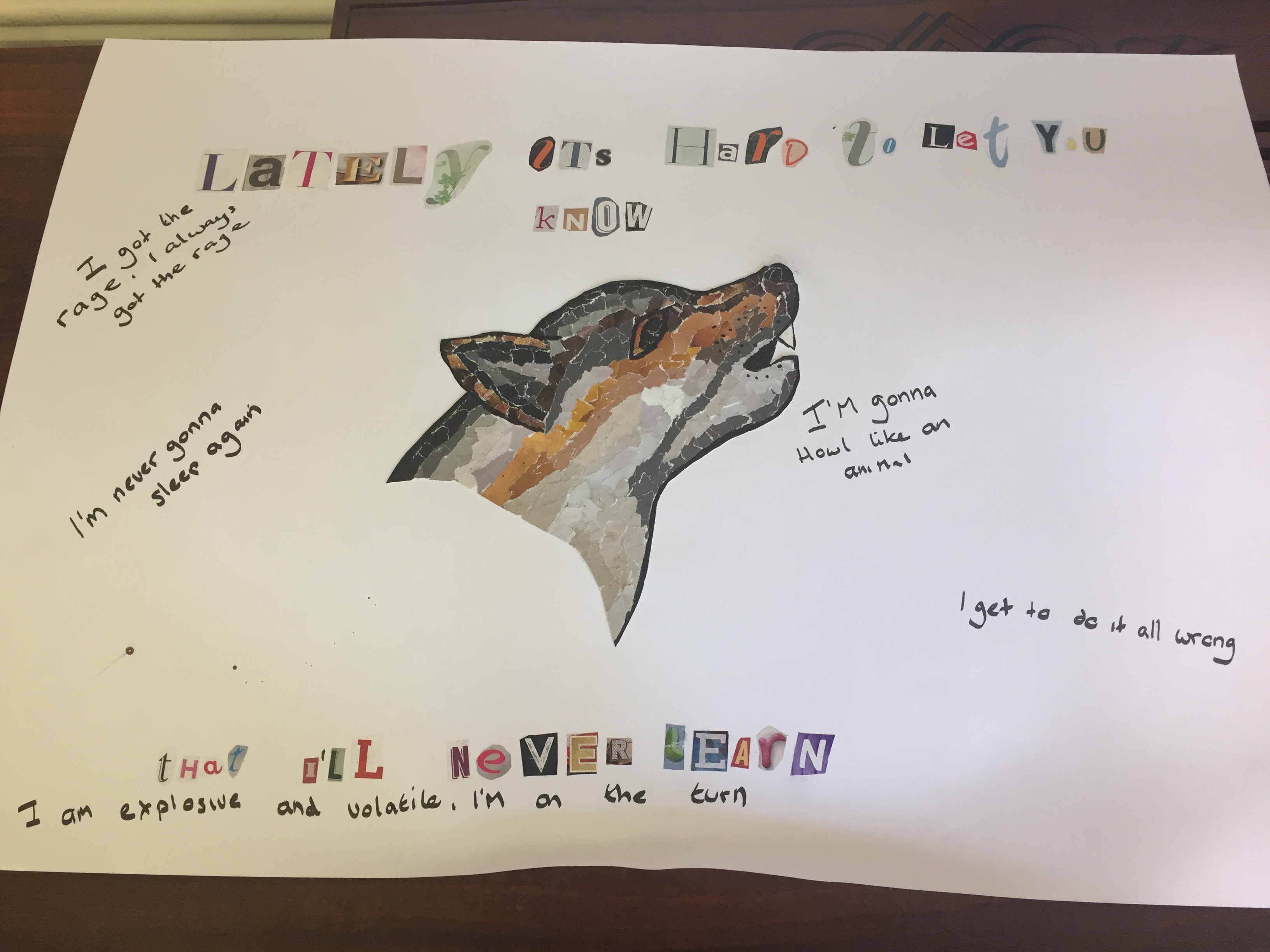
We’ve tried talking, we’ve asked for and begged for help, we’ve called the helplines, the crisis lines, we’ve been to A&E, walked until our shoes wore out, coloured in our colouring books, we’ve drunk more tea than we can count, and we’ve had a fucking bath. We do all the things we’re told because otherwise we get labelled as difficult or told we don’t really want help; since the pandemic started, the already stretched services are at breaking point. There is no one to talk to.
The messages are well-meaning, but there is a limit to what helplines can do, and even being in contact with services doesn’t guarantee support. In the last two years, three people I know have taken their lives, and all three were known to services. Being told to talk didn’t help them; awareness couldn’t save them. They had all tried talking; they had all tried reaching out.
In less than two weeks, it’ll be two years since Juliette died.
This is why I don’t like awareness campaigns; they’re meaningless, hollow gestures with no real purpose or motive that don’t address the real problems or try to change the systemic problems with mental health services.
Please don’t tell me to reach out, talk or ask for help. I’ve done it for so long, and I’m tired now.
For Nancy, for Juliette, for Ella.