I was trying to explain to someone recently the conflicting feelings that come into my head around self-harm. I want to self-harm, but really, I don’t. I keep thinking how much better it was to have an outlet for the way I feel, but really, I know that it wouldn’t help, it didn’t help, not really, not properly. But that doesn’t stop my mind jumping to it when I’m stressed, anxious or overwhelmed.
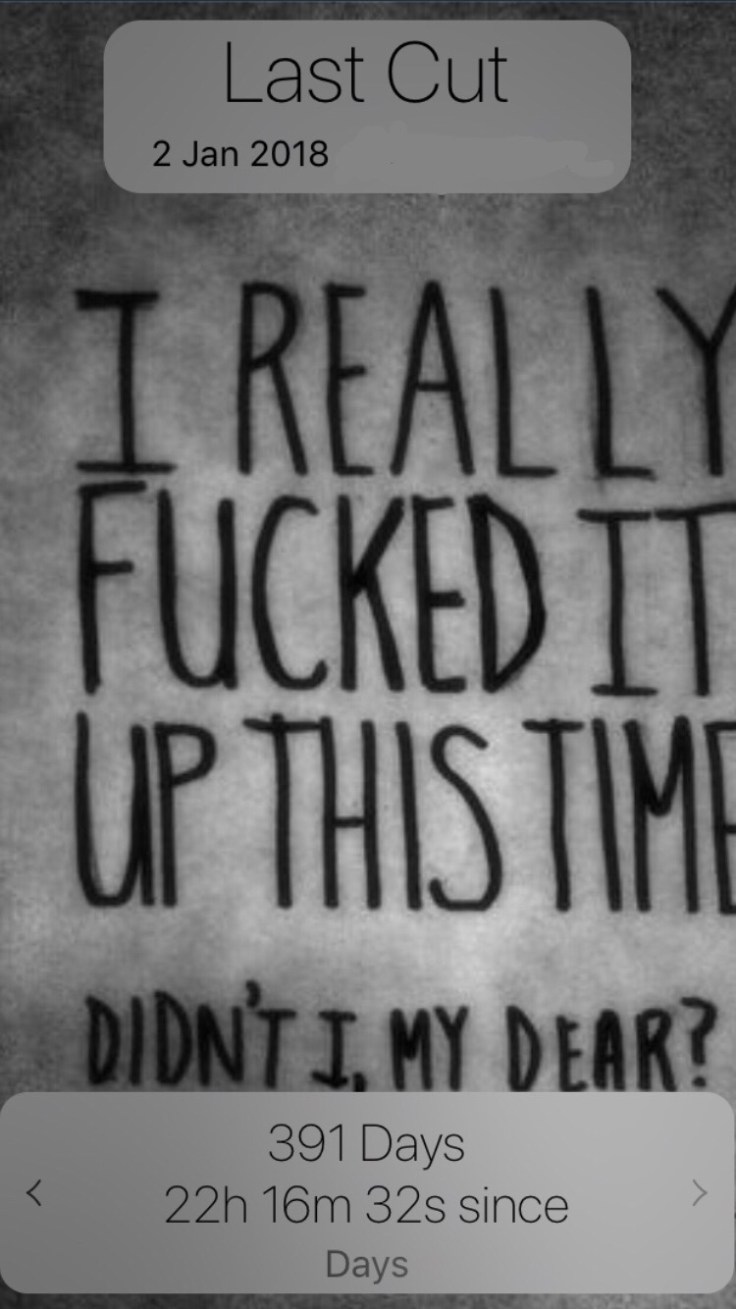
I haven’t self-harmed in 391 days, but I self-harmed from the age of 17 to 32 and intermittently before that. It’s not that I want to self-harm, it’s just that I want to breathe and not feel like I’m suffocating. I want to stop feeling like I’m dragging a weight around with me or wading through custard, and when it’s been something I’ve done for so long, it’s an immediate thought, an ingrained reaction that my mind jumps to when I feel bad.
I’m not naive, I know that just because I haven’t self-harmed in a long time, it doesn’t mean I won’t ever do it again. I can’t say for sure that I know I’ll never self-harm again, and even now, it’s not that I never do anything unhealthy/ potentially harmful or things that could be seen as negative ways of managing things, they’re just less destructive and don’t involve me ending up in A&E. The longer time goes on the bigger the stakes, once I was past 6 months I’d beat my previous longest time, then it was 7 months, 9 months and finally a year.
Sometimes people ask what they can do to help or make things easier, but I don’t always want them to do anything other than listen or try to see things from my position. I know some people are more practical than others, and their reaction is to look for a solution, but sometimes the solution is just to please listen to me and hear what I’m saying when I say how overwhelmed and stressed I feel. That I miss people I was close to, how alone I feel, how the light at the end of the tunnel feels very dim and distant right now, that’s what can be done to help.
Sometimes I just want someone to take me down to the car park and let me cry